Summary
Neisseria meningitidis, commonly known as meningococcus, can colonize the mucous membranes of the nasopharynx in healthy individuals, where it may exist harmlessly without any signs or symptoms. However, under certain conditions, this bacterium can lead to potentially life-threatening conditions such as meningitis, pneumonia, and sepsis [1].
Neisseria meningitidis, commonly known as meningococcus, can colonize the mucous membranes of the nasopharynx in healthy individuals, where it may exist harmlessly without any signs or symptoms. However, under certain conditions, this bacterium can lead to potentially life-threatening conditions such as meningitis, pneumonia, and sepsis [1].
Staining and Microbiologic Features:
- Gram-negative aerobes [2]
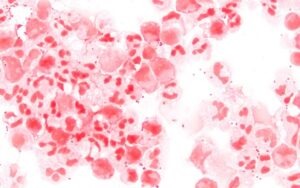
Neisseria meningitidis CSF Gram 1000” by Microman12345 is licensed under CC BY-SA 4.0.
- Kidney bean-shaped cocci in pairs (diplococci) [3]
- Can ferment maltose (Neisseria gonorrhoeae does not ferment maltose). [2]
- Shows its best growth on chocolate agar [4]
- Thayer-Martin VCN agar, which includes vancomycin, colistin, and nystatin, serves as a culture medium for Neisseria. These antibiotics inhibit the growth of competing bacteria (vancomycin against gram-positive organisms, colistin against gram-negative organisms, and nystatin against fungi) and create a selective environment that promotes the growth of Neisseria. [4]
Virulence:
- Neisseria meningitidis uses its pili to attach to the nasopharynx. [5]
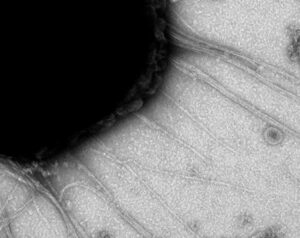
Neisseria meningitidis pili” is licensed under CC BY 4.0.
- Neisseria meningitidis have a polysaccharide capsule that shields them from phagocytosis unless specific antibodies are present to coat (opsonize) them [5]. The polysaccharide capsule composition serves as the basis for classifying Neisseria meningitidis into diverse serogroups, which encompass A, B, C, D, E, H, I, K, L, X, Y, Z, and W-135 [5]. This capsule is absent in Neisseria Gonorrhoeae [6].
- Some disease-causing meningococci can also lyse IgA antibodies by producing IgA1 protease [5].
- It can also release LPS/endotoxin [5].
- N. meningitidis has also developed an acquisition system to extract iron from the host [5].
- Neisseria can elude the host’s defense mechanisms through antigenic variations resulting from the genetic recombination of pili genes or the expression of diverse Opa proteins [7].
Transmission:
- Some people are asymptomatic carriers of Neisseria meningitidis [5].
- It can colonize the nasopharynx or oropharynx and spread through respiratory secretions [5,8].
Susceptible Population:
- Infants: During the initial months (usually around six months), infants rely on maternal antibodies for protection, as their own immune systems take time to develop completely. Therefore, the child is highly susceptible to infection from six months to two years of age [5].
- College students and army recruits in close living conditions.
- Asplenia: The lack of spleen increases susceptibility to Neisseria meningitidis infection due to diminished phagocytic function and decreased antibody production [9].
- Patients with Terminal complement deficiencies: C5-C9 are involved in the formation of membrane attack complex [10].
Diseases:
- Meningitis: Serogroups A, B, and C usually cause meningitis [5]. Presentation: Confusion, lethargy, fever, headaches, nausea, vomiting, increased sensitivity to light, neck stiffness, presence of Kernig and Brudzinski signs [11].
- Waterhouse Fridreichsen syndrome: In Waterhouse-Friderichsen syndrome, there is acute adrenal insufficiency due to meningococcemia and bilateral adrenal hemorrhage.

File: Waterhouse-Friderichsen. IMG 2912.jpg” by Amadalvarez is licensed under CC BY-SA 4.0.
The affected patient can present with petechial rash, low blood pressure, DIC, or shock [12]. Endotoxins/lipopolysaccharides released from the bacteria play a role in this hemorrhaging process [5].
- Meningococcemia: Occurs when the Neisseria enters the bloodstream and multiplies, resulting in rapid dissemination and systemic infection. The patient can present with chills, elevated body temperature, rash, and muscle pain [5].
Diagnostic Testing:
- Lumbar puncture to get a CSF specimen. Gram staining and culture of CSF. [4,11,13]
- Do a CT scan before obtaining the CSF specimen if there is a high suspicion of space-occupying lesion or focal neurologic deficits. [4,11,13]
- Blood cultures [4,11,13]
- CSF analysis will show decreased glucose levels and elevated levels of neutrophils and protein. [11,14]
References:
1 Medical Microbiology by Patrick R. Murray Ph.D., Ken Rosenthal Ph.D., Michael A. Pfaller MD, 8th edition (page no: 235)
2 First Aid for USMLE step 1, 2021 edition (page no: 141)
3 CMMRS edition 6, 2016-17 (page no: 64)
4 CMMRS edition 6, 2016-17 (page no: 66)
5 CMMRS edition 6, 2016-17 (page no: 65)
6 First Aid for USMLE step 1, 2021 edition (page no: 142)
7 Robbins & Cotran Pathologic Basis of Disease, 10th Edition (page no: 365)
8 Robbins & Cotran Pathologic Basis of Disease, 10th Edition (page no: 364)
9 Robbins & Cotran Pathologic Basis of Disease, 10th Edition (page no: 629)
10 Robbins & Cotran Pathologic Basis of Disease, 10th Edition (page no: 242)
11 Step-Up to Medicine, 6th edition (page no: 373)
12 Robbins & Cotran Pathologic Basis of Disease, 10th Edition (page no: 1122)
13 Step-Up to Medicine, 6th edition (page no: 374)
14 First Aid for USMLE step 1, 2021 edition (page no: 180)

