Summary
Common diabetes medications include metformin, which decreases glucose production in the liver and improves insulin sensitivity, making it a first-line treatment for type 2 diabetes. Sulfonylureas, like glipizide, stimulate the pancreas to release more insulin. DPP-4 inhibitors, such as sitagliptin, help prolong the action of incretin hormones, which increase insulin release and decrease glucagon levels. GLP-1 receptor agonists, like exenatide, mimic incretin hormones to enhance insulin secretion and promote satiety. SGLT2 inhibitors, such as empagliflozin, work by preventing glucose reabsorption in the kidneys, leading to its excretion in urine. Insulin therapy, critical for type 1 diabetes and sometimes necessary for type 2, involves various forms, including rapid-acting, long-acting, and intermediate-acting insulins to maintain blood glucose levels.
Note: the listing of the drugs below is not a prescription for anyone. Taking diabetes medication without a doctor’s prescription can be fatal.
Type 1 Diabetes Mellitus
- Usually young patients. 40% are lesser than 10 years of age.
- Polyuria, polydipsia, weight loss
- Random blood glucose levels of 200 mg/dL (11.1 mmol/L) or more.
- Fasting blood glucose levels of 126 mg/dL (7.0 mmol/L) or more. Documented more than once.
- Ketonemia, ketonuria, or both.
- Islet antibodies usually identified.
Type 2 Diabetes Mellitus
- Fewer or no symptoms.
- Usually 40 years of age or above. (Age for developing type 2 DM is reducing.)
- Polyuria, polydipsia.
- Many women will present with candida vaginitis. (Glucose in urine promotes candida growth.)
- Fasting blood glucose levels of 126 mg/dL (7.0 mmol/L) or greater. Documented more than once.
- 75 g oral glucose tolerance test giving 200 mg/dL (11.1 mmol/L) or more after two hours is diagnostic. (Most sensitive test.)
- HbA1c is 6.5% or more.
- Usually, the patient has associated diseases like hypertension, dyslipidemias, and atherosclerosis.
Medications
Drugs are broadly classified into the following categories:
- Drugs that reduce glucose absorption (acarbose, miglitol)
- Drugs that reduce internal glucose production (metformin)
- Drugs that throw glucose out of the body using the kidneys (SGLT2 inhibitors, canagliflozin, dapagliflozin, empagliflozin)
- Drugs that directly or indirectly increase the insulin levels (sulfonylureas, meglitinide analogs, D-Phenylalanine derivatives, DLP1 agonists, and DPP4 inhibitors.)
- Drugs that make peripheral tissue insulin sensitive (rosiglitazone, pioglitazone)
- Insulins
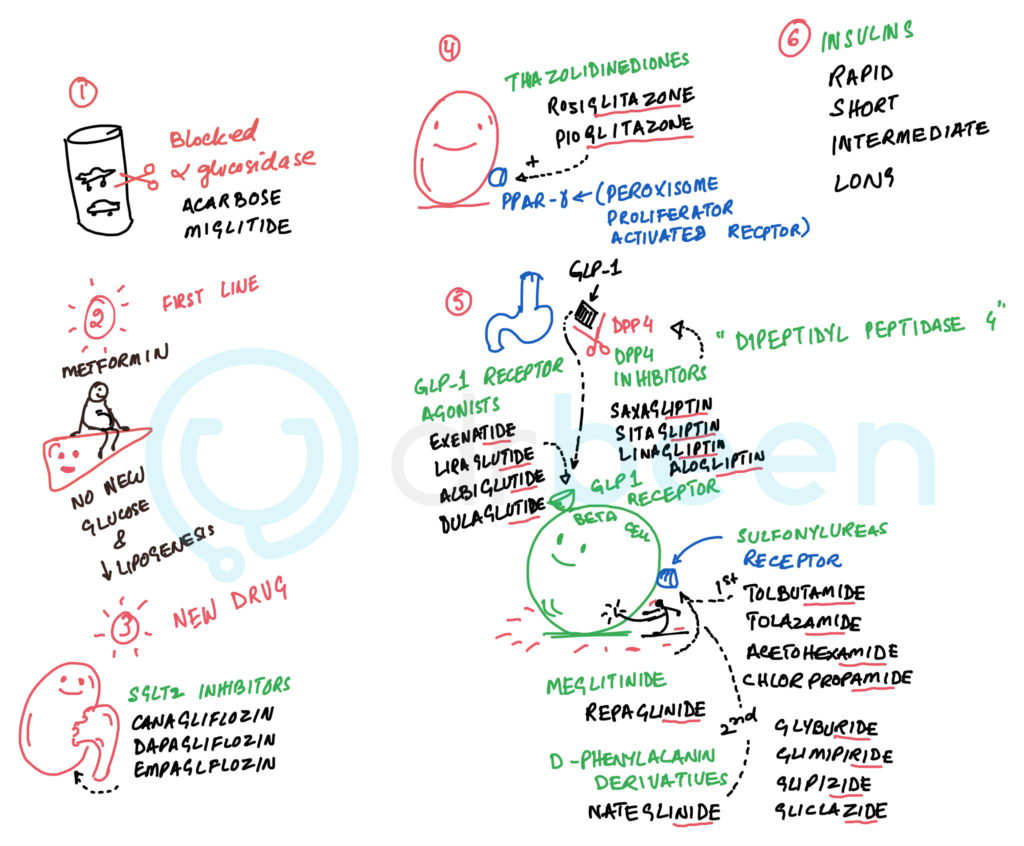
Figure: drug names in various categories
List of Drugs
- Medicines that Affect Glucose Absorption
- Acarbose and Miglitol
- Competitive inhibitors of the alpha-glucosidase enzyme in the gut. This enzyme digests starches. Hence, glucose digestion and absorption reduces.
- Cause flatulence.
- Acarbose and Miglitol
- Glucose Lowering Agents (act on the liver, muscle, or adipose tissues.)
- Metformin (first line)
- Increases hepatic protein kinase (PK) activity by increasing adenosine monophosphate levels (AMP). This, in turn, reduces hepatic gluconeogenesis and lipogenesis.
- 1.5h to 3h half-life. Excreted unchanged by the kidneys.
- Improves hyperglycemia and hypertriglyceridemia in obese patients without weight gain.
- In the US metformin is contraindicated at the creatinine levels of 1.4 mg/dL in women and 1.5 mg/dL in men.
- Most common side effects are gastrointestinal (anorexia, nausea, vomiting, abdominal discomfort, and diarrhea.)
- Therapeutic doses do not cause hypoglycemia. Hence this drug is called euglycemia or antihyperglycemic drugs instead of a hypoglycemic drug.
- Can cause vitamin B12 deficiency by interfering with its absorption.
- Lactic acidosis has been reported.
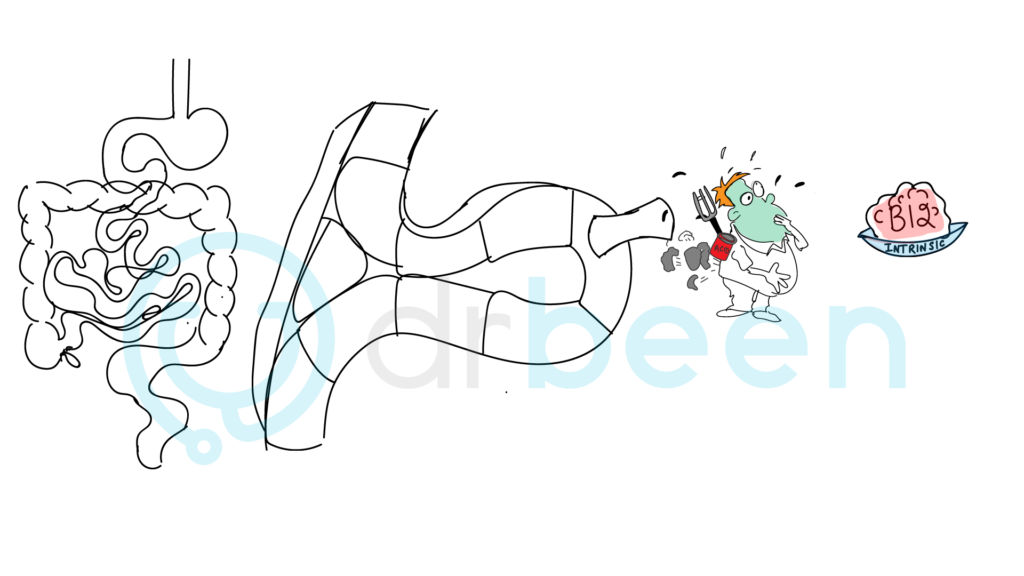
- Figure: metformin blocking B12 absorption. Keep in mind that vitamin B12 deficiency can occur with long-term metformin use.
- Metformin (first line)
- Beta cell stimulants (to trigger insulin release)
- Sulfonylureas (bind to sulfonylureas receptors on the surface of the beta cells.)
- First generation: Tolbutamide, Tolazamide, Acetohexamide, Chlorpropamide.
- Second generation: Glyburide, Glipizide, Gliclazide, Glimipiride.
- More potent than the first generation. Use with caution in patients in whom prolonged hypoglycemia can be dangerous e.g. elderly or heart patients.
- Glyburide has the most affinity and Tolbutamide has the least affinity.
- Binding to the sulfonylureas receptors closes K+ channels resulting in the cell depolarization and insulin release.
- Used in type 2 because these drugs need functioning beta cells.
- Meglitinide Analogs
- Repaglinide
- Binds to the sulfonylureas receptors, closes the ATP sensitive K+ channels, depolarizing the beta cells and releasing insulin.
- Repaglinide
- D-Phenylalanine Derivatives
- Nateglinide
- Binds to the sulfonylureas receptors, closes the ATP sensitive K+ channels, depolarizing the beta cells and releasing insulin.
- Nateglinide
- Sulfonylureas (bind to sulfonylureas receptors on the surface of the beta cells.)
- Incretins (trigger insulin release)
- GLP-1 receptor agonists
- Exenatide, liraglutide, albiglutide, dulaglutide.
- Rapidly proteolyzed by dipeptidyl peptidase 4 (DPP4) and other enzymes.
- Oral glucose causes the release of gut hormones glucagon-like peptide 1 (GLP1) and glucose-dependent insulinotropic polypeptide 1 (GIP1).
- These hormones increase glucose-induced insulin release.
- In type 2 DM these hormones are reduced.
- Exenatide, liraglutide, albiglutide, dulaglutide.
- DPP4 Inhibitors
- Sitagliptin, Saxagliptin, Linagliptin, Alogliptin
- GLP-1 receptor agonists
- Thiazolidinediones
- Sensitize peripheral tissue to insulin.
- Rosiglitazone and pioglitazone.
- Acts on the peroxisome proliferator-activated receptor gamma (PPAR-gamma) resulting in liponectin increase and resistin reduction.
- Rosiglitazone is reported to increase the risk of angina pectoris and myocardial infarction (MI). Banned in Europe.
- 3-4% patients get edema.
- Contraindicated in NY Heart Association class III and IV cardiac status.
- Increases risk of fractures in women is reported (not men.)
- 4% patients developed anemia. (Maybe dilutional due to the fluid retention.)
- Weight gain possibly fluid retention as one factor.
- Long-term pioglitazone administration needs consideration for the risk of bladder cancer.
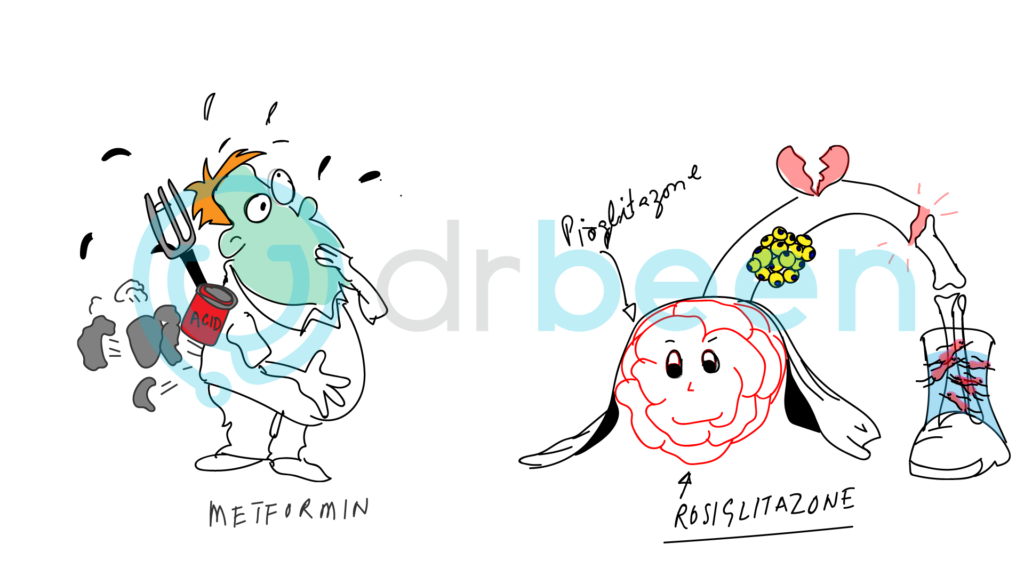
Figure: A pious (pioglitazone) rose (rosiglitazone) met a former (metformin).
Remember metformin by the character on the left. He is nauseated, bloated, and has a lactic acid box. Some of the side effects of metformin.
For pioglitazone and rosiglitazone see how the rose is on a broken bone (stem) this is to help you remember that fractures can occur. See the broken heart to help you remember that angina pectoris and myocardial infarction risk increases. The boat filled with fluids is for water retention which in turn is causing dilutional edema – see the RBCs swimming in this extra fluid.
The yellow fat cells attached to the stem should help you remember that these drugs work on PPAR-gamma receptors to help increase liponectic and reduce resistin.
- Na+/Glucose Co-Transport Inhibitors (SGLT2 Inhibitors)
- Canagliflozin, Dapagliflozin, Empagliflozin
- Canagliflozin reduces glucose threshold from ~180 mg/dL to 70-90 mg/dL.
- Causes glycosuria.
- Modest weight loss.
- Reduces HbA1c by 0.6% to 1%.
- Insulins
- Rapid-acting
- Apidra, Novolog, Humalog
- Short-acting
- Regular Insulins (Novolin, Humulin)
- Intermediate-acting
- NPH Insulins
- Long-acting
- Detemir, Glargin
- We will discuss these in detail in another post
- Rapid-acting

