Summary
Some species of Shigella include Shigella dysenteriae, Shigella flexneri, Shigella boydii, and Shigella sonnei. Shigella sonnei is responsible for most Shigella infections in the United States. S. flexneri's prevalence shifts geographically, with a higher burden noted in developing nations. S. dysenteriae, though less frequent, can erupt in epidemic waves. [1]
Some species of Shigella include Shigella dysenteriae, Shigella flexneri, Shigella boydii, and Shigella sonnei. Shigella sonnei is responsible for most Shigella infections in the United States. S. flexneri’s prevalence shifts geographically, with a higher burden noted in developing nations. S. dysenteriae, though less frequent, can erupt in epidemic waves. [1]
Staining and Microbiologic Features:
- Gram-negative bacilli [2].
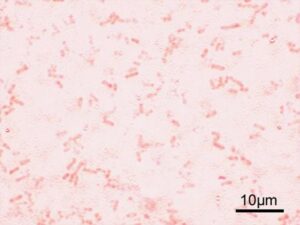
Shigella flexneri Gram” by Y tambe is licensed under CC BY-SA 3.0
- Shigella’s exclusive reservoir is humans [1].
- It does not produce H2S [2].
- S. dysenteria is a non lactose fermenting organism [3].
- Shigella displays glucose fermentation. With the exception of Shigella sonnei, other Shigella species do not exhibit lactose fermentation [4].
- Shigella is acid-resistant, enabling it to survive the acidic conditions of the stomach and reach the intestines, where it can cause infection. Consequently, Shigella requires a smaller infective dose to initiate an infection in the intestines [2]
- In contrast to Salmonella infection, antibiotic therapy in treating Shigella infection reduces the duration of Shigella excretion in feces [2].
- The presence of IgA antibodies directed against Shigella confers protection from Shigella infection [5].
- Shigella is not a component of normal intestinal flora. [6]
Virulence and Pathogenicity:
- Shigella utilizes M cells, specialized epithelial cells in the gastrointestinal tract, to facilitate entry into the mucosal tissue and initiate infection. [2]
- Shigella uses its type III secretion system to secrete Ipa proteins (such as IpaA, IpaB, IpaC, and IpaD) into the host’s epithelial cells and macrophages. By interacting with the host cell membrane, these proteins promote the engulfment of Shigella [1].
- Shigella disrupts the phagocytic vacuole, enabling replication in the host cell cytoplasm.
- Shigella rearranges the host cell’s cytoskeleton (actin filaments). This allows Shigella to move through the cytoplasm and pass from one host cell to another. The ability of Shigella to spread directly between host cells contributes to its pathogenicity and evasion of immune responses [1].
- Inflammatory mediators, such as IL-1β, released during apoptosis of host cells in response to Shigella infection recruit neutrophils. This neutrophil infiltration weakens the intestinal barrier, potentially facilitating Shigella’s deeper tissue invasion [1].
- S. dysenteriae is a non-motile pathogen as it lacks flagella and, consequently, tests negative for the H antigen. [3]
- S. dysenteriae produces Shiga toxin. This toxin disrupts protein synthesis by inactivating the 60S subunit of ribosomes, leading to cell death and tissue damage. [6]
Transmission:
- Transmission primarily occurs through the fecal-oral route [3], with Shigella spreading through contaminated food and water consumption. Person-to-person transmission is frequent, and flies can indirectly transmit Shigella by carrying it from feces to contaminate food or surfaces [2].
Diseases and Complications:
- Bacillary Dysentery: The patient can present with fever, tenesmus, abdominal pain, and bloody diarrhea [2,7].
- Hemolytic Uremic Syndrome: Shiga toxin produced by shigella can damage the glomeruli, resulting in hemolytic uremic syndrome. The affected patient may present with a triad of symptoms, including hemolytic anemia, thrombocytopenia, and kidney injury.
Diagnostic Testing:
- Stool culture [8]
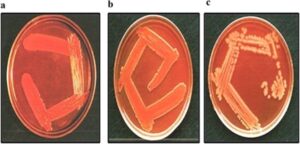
File:Shigella-culture.png” by Prakash R1, Bharathi Raja S, Devaraj H, Devaraj SN. is licensed under CC BY 4.0.
- Nucleic Acid Amplification Tests (NAATs) [8]
References:
1 Medical Microbiology by Patrick R. Murray Ph.D., Ken Rosenthal Ph.D., Michael A. Pfaller MD, 8th edition (page no: 260)
2 First Aid for USMLE step 1, 2021 edition (page no: 144)
3 CMMRS edition 6, 2016-17 (page no: 84)
4 Jawetz, Melnick, & Adelberg’s Medical Microbiology Twenty-Seventh Edition (page no: 237)
5 CMMRS edition 6, 2016-17 (page no: 85)
6 CMMRS edition 6, 2016-17 (page no: 76)
7 Medical Microbiology by Patrick R. Murray Ph.D., Ken Rosenthal Ph.D., Michael A. Pfaller MD, 8th edition (page no: 261)
8 Jawetz, Melnick, & Adelberg’s Medical Microbiology Twenty-Seventh Edition (page no: 238, 239)

